The Navy released a new set of COVID-19 guidelines Wednesday to standardize the fleet’s response to the pandemic and establish a framework for commanders to use as the Pentagon moves toward resuming full operations.
The Navy’s policy, which includes detailed definitions of terms and suggested mitigation efforts, was released a day after Secretary of Defense Mark Esper lifted existing movement restrictions and pushed COVID-19-related conditions-based operational decisions to service chiefs and combatant commanders.
The Navy’s new guidelines make it apparent the service is assuming it will be operating under the threat posed COVID-19 spread for a long time.
“Our forces continue to operate forward every day – the impact of COVID-19 on the global community only heightens the critical role our Navy plays in maintaining security and stability at sea,” Vice Adm. Phillip Sawyer, the Navy’s operations chief in charge of coordinating the service’s response to COVID, said in a statement. “As we learn more about this virus, the Navy will continue to take steps necessary to preserve our operational readiness while protecting the health of our forces.”
The guidance, released by Sawyer in a NAVADMIN, is biased toward trying to limit the spread of COVID-19 in the shipboard environment, but it also applies to all personnel and units, including reservists scattered around the country.
The Navy’s new guidance comes as the Department of Defense Inspector General conducts a review of procedures the Navy already put in place to respond to COVID-19 outbreaks on ships. In March, USS Theodore Roosevelt (CVN-71) pulled into Guam with dozens of COVID-19 cases. During the following two months, more than 1,000 crew members tested positive as the carrier remained sidelined from deployments.
In April, USS Kidd (DDG-100) flew two sick sailors ashore and transferred others to be treated aboard amphibious ship USS Makin Island (LHD-8). Kidd curtailed its deployment and pulled into San Diego, where the crew left the ship and the ship was disinfected. Before the Navy stopped reporting numbers from the destroyer, there had been 78 sailors who tested positive for COVID-19.
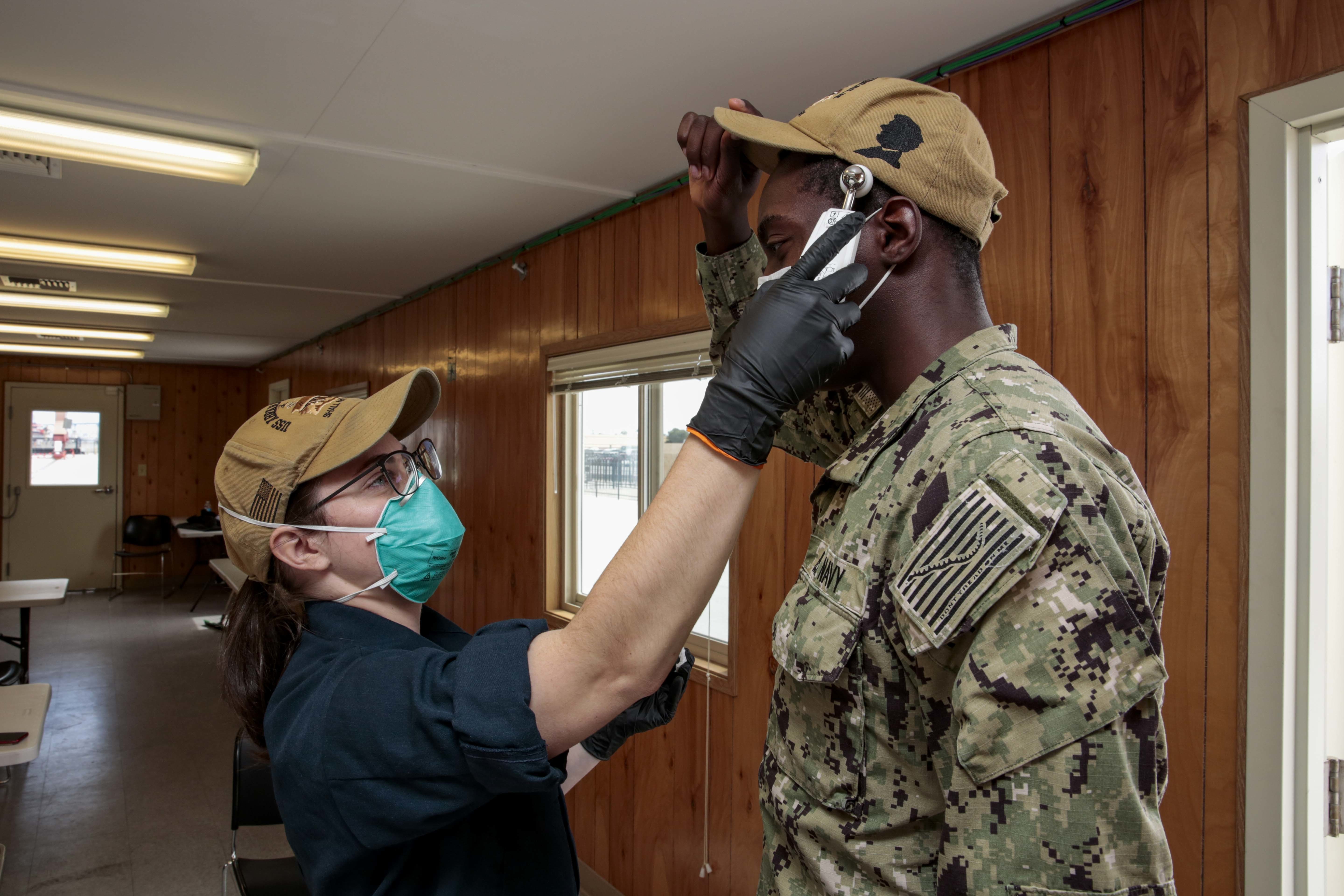
Deploying units are required to conduct medical screening of all crew members, go through a minimum 14-day Restriction of Movement (ROM) sequester, and continue frequent hand-washing and wearing face coverings while underway, according to the Navy.
The Navy’s strategy to limit the spread of COVID-19 hinges on creating a bubble, which the NAVADMIN defines as “U.S. Navy term for individuals, units or installations that have established low probability of COVID-19 infection. A crew that has been underway, or ROM-sequestered at the pier, for greater than 14 days without COVID-19 positive personnel and no COVID-19 symptoms is within a bubble.”
The NAVADMIN defines a ROM-sequester as “U.S. Navy term for preemptive separation of forces to reduce risk of infection while establishing a COVID-free bubble. ROM-sequester can be conducted onboard ship, in contracted facilities, or in personal residence dependent on unit-specific scenarios. During ROM-sequester, interaction with individuals traveling outside of the ROM-sequester location must be minimized. Interaction within ROM-sequester location is restricted to basic necessities such as food delivery.”
The Navy employed the bubble strategy with the Nimitz Carrier Strike Group. All crew members of USS Nimitz (CVN-68) spent most of April isolated before the carrier left Bremerton, Wash., earlier this month. Likewise, the carrier air wing and the CSG’s escorts were isolated in San Diego ahead of linking up with the carrier. The Navy tested all 8,000 sailors before boarding their ships.
While COVID-19 testing is the only way to identify asymptomatic individuals, the Navy recognizes testing will not guarantee deploying units will remain COVID-19 free. The NAVADMIN details actions commands take when a crew member exhibits COVID-19 symptoms, tests positive and recovers.
“Personal responsibility and disciplined organizational public health protection measures are the bedrock of risk reduction and risk mitigation,” Rear Adm. Bruce Gillingham, the Navy’s Surgeon General, said in a statement.
The following definitions are among the COVID-19 terms detailed in the NAVADMIN released by Vice Adm. Phillip Sawyer:
Patient (or Person) Under Investigation (PUI): An individual with signs or symptoms of COVID-19 who has a test result pending or would have been tested had a test been available. Members are no longer a PUI when they: a) receive a negative COVID-19 lab test result; or, b) have met all criteria for return to work in paragraph 7.d. Asymptomatic individuals quarantined due to close contact with a COVID positive member are not classified PUI. Asymptomatic individuals being tested for COVID-19 are not considered PUIs while awaiting test results.
Close Contact: Individuals identified as being within approximately 6 feet (2 meters) of a COVID-19 case for a prolonged period of time (more than 15 Minutes). Close contact can occur while caring for, living with, visiting, working with, or sharing a densely populated space with a COVID-19 case. Close contact can also be established via direct contact (e.g., being coughed or sneezed upon by a COVID-19 case). Determination of close contact presumes the interaction transpired during the COVID-19 Cases potentially infectious period currently defined as 48 hours prior to symptom onset (or positive test if asymptomatic) to the time the COVID-19 case is placed in isolation. Some examples specific to the shipboard environment include: a) individuals within the COVID-19 cases berthing area assigned an adjacent rack including directly across a narrow aisle; b) prolonged interaction within relatively confined spaces internal to the ship (e.g., work space, galley, gym, smoking deck, chapel, etc.).
Medical screening: COVID-19 medical screening should include evaluation for both typical and atypical symptoms. Typical symptoms of COVID-19 include: cough, shortness of breath or difficulty breathing, fever, chills, muscle pain, gastrointestinal distress, and recent loss of taste or smell. Atypical symptoms of COVID-19 include, but are not limited to: sore throat, rhinorrhea (runny nose), nasal congestion, nausea, diarrhea, headache, increased confusion, dizziness, and malaise. The CDC has a list of COVID-19 symptoms.
Bubble: U.S. Navy term for individuals, units or installations that have established low probability of COVID-19 infection. A crew that has been underway, or ROM-sequestered at the pier, for greater than 14 days without COVID-19 positive personnel and no COVID-19 symptoms is within a bubble.
Bubble to Bubble Transfer (B2BT): U.S. Navy term for movement of units or personnel from one bubble to another via controlled means. A wide variety of modes/means of transportation can be used for B2BT. The key factor is that the evolution is closely controlled to minimize risk of COVID-19 exposure.
Pre-Deployment Screening: Will consist of an assessment of COVID-19 exposure history, a temperature check, a check for COVID-19 signs and symptoms listed in para 2.e, review of any past COVID-19 testing and a thorough evaluation of the members high-risk factors.





